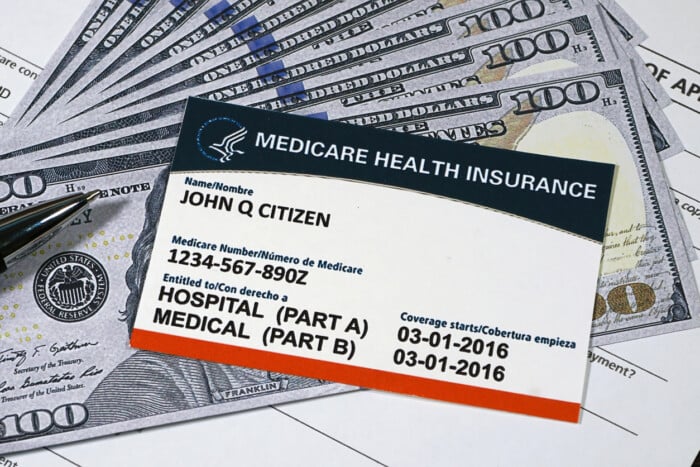
Major changes are coming to Medicare plans in 2025, with experts warning seniors that staying on the same plan could result in financial loss. The open enrollment period, which began on October 15 and runs through December 7, is unfolding amid significant confusion as premiums, benefits, provider networks, and prescription costs are being substantially altered. Seniors are urged to use the official Medicare.gov Plan Finder to compare local options before making decisions.
Even with a potential federal government shutdown, essential Medicare functions — including enrollment and medical coverage — will continue uninterrupted.
According to analyses by the Wall Street Journal and health insurance experts, several key changes will directly affect beneficiaries next year.
Many insurance providers are shifting costs to consumers as part of cost-cutting measures. Some plans will raise hospital copays from $395 per day to $550, while previously zero-premium plans may now charge around $48 per month. Policyholders are encouraged to review all notices regarding changes to their benefits and coverage.
Roughly 1.2 million Medicare Advantage enrollees are expected to lose access to their current plans. Insurers are scaling back PPO plans that allow flexible hospital choice and expanding HMO networks that limit which hospitals are covered. Some hospitals are even withdrawing from the Medicare Advantage network altogether. Out-of-network care may be uncovered under HMO plans, making it essential to confirm coverage in advance.
Sarah Murdoch, director at the Medicare Rights Center, advised enrollees to “always confirm directly with hospitals and clinics,” as insurer network listings can be inaccurate.
Prescription coverage is also narrowing. The number of standalone Part D drug plans will drop from 709 in 2024 to 360 by 2026, nearly a 50% reduction. Deductibles and co-insurance rates are also rising, increasing out-of-pocket expenses for many. Experts recommend using the Plan Compare tool to evaluate Advantage plan drug coverage and check for Medigap supplemental insurance compatibility.
Additional perks such as grocery credits, gym memberships, and health item subsidies — once aggressively expanded by insurers to attract members — will be scaled back next year.
Beneficiaries can seek one-on-one counseling through each state’s State Health Insurance Assistance Program (SHIP), which provides trained volunteers to help compare plans and navigate the enrollment process. Experts emphasize that comparing only premiums is risky. Seniors should first determine which factors — such as medical costs, drug prices, or provider convenience — matter most to them before choosing a plan to avoid potential losses.
BY HANKIL KANG [kang.hankil@koreadaily.com]

![Tesla Diner loses buzz six months after splashy opening in Hollywood Around noon on February 13, the Tesla Diner appears relatively quiet. [Sangjin Kim, The Korea Daily]](https://www.koreadailyus.com/wp-content/uploads/2026/02/0218-Tesla-1-100x70.jpg)
![Social media users who post ICE enforcement updates could face subpoenas A community member records with their phone as federal immigration agents conduct immigration enforcement tasks in Minneapolis, Minnesota, U.S., February 5, 2026. [REUTERS]](https://www.koreadailyus.com/wp-content/uploads/2026/02/0218-ICE-Minneapolis-100x70.jpg)
![U.S. arrivals face hourlong immigration waits at Incheon Airport Incheon International Airport’s Terminal 2 is crowded with arriving passengers on Jan. 30. [Courtesy of reader]](https://www.koreadailyus.com/wp-content/uploads/2026/02/0217-Incheon-100x70.jpg)
